Regenerative Medicine
By: Cynthia Adams | Photos by: Nancy Evelyn
The cure for bad breaks: a putty like no other
As I write this, my black and blue pinky toe is “buddy taped” to the neighboring toe. A broken toe is one of the most common of all fractures, but the least consequential. But a fracture is a bad break in every sense of the word:
Artist William Mangum was cleaning the gutters of his new home when the ladder listed to the right and he landed on the deck, shattering bones in his shoulder and elbow. The injuries meant he could not resume painting for six months of recovery time
With his mind on the good times he was about to enjoy, James Catlett climbed out of his car to join a family reunion in McCall, South Carolina. He lost his footing and fell hard onto the curbing. As searing pain tore through his hip, the senior already suspected the worst: a broken hip.
They suffered in good company. Statistically, we accident-prone humans average two fractures in a lifetime.
Fractures are the most common orthopedic emergency, affecting as many as seven million people annually. The direct costs of medical treatment for broken bones in the United States are estimated between $17-18 billion annually. Many fractures simply do not heal, regardless of conventional treatment.
Worst of all, in wartime, fractures often force amputation.
What if an injection could resolve a break in days, rather than weeks? At UGA, studies with pigs and sheep will lead the way to a revolutionary change with regenerative medicine. Regenerative medicine means restorative treatments that shave weeks or more off of traditional treatment.
Two UGA alums, Jennifer Mumaw and Erin Jordan, are members of a multi-university research project in regenerative medicine, one of vast significance for fracture victims.
In 2008, researchers at Baylor and Rice began developing something extraordinary. The idea afoot was to devise a substance that could be injected into fractures with the power to heal them in only days. The work wound up being translated into action by a team at UGA’s Regenerative Bioscience Center under the direction of Steve Stice, professor and GRA Eminent Scholar in animal science and John Peroni, a professor of large animal medicine.
The Regenerative Bioscience Center received Department of Defense funding through a Baylor Medical School to work in tandem with the other research universities. In cooperation with one another, they developed a surgical putty, or gel, to be surgically injected and molded to repair broken bones. The translucent substance more closely resembles a gel, although researchers refer to it as putty. Once injected, it starts releasing powerful proteins that initiate bone formation using the animal’s own cells.
The full required healing time? Three weeks.
“Baylor and Rice, and other institutions, did much of the initial research. Baylor developed the virus and Rice developed the polymer,” explains post-doctoral UGA researcher Jennifer Mumaw, who has recently begun veterinary studies. ”They have been integral parts of the process.” According to Mumaw and her team member, Erin Jordan, preliminary gene therapy was done at Baylor and the development of the experimental substance was done at Rice.
Mumaw has published articles with highly detailed scans of the hydrogel that is also known to the researchers involved as “fracture putty.” The injectable putty immediately jumpstarts rapid healing.
“It feels like a gel and it’s called ‘micro-encapsulation’,” she says. “Microscopically, it looks like round circles. In reality it is a billion of these circles with cells on the inside—a circle of jelly with cells.” The injected putty rapidly increases the natural rate of bone healing in the region of the fracture.
The stem cell methodologies to create the gel are crucial. “We used sheep stem cells,” says Mumaw, who holds two UGA degrees, a BS and PhD, and has worked on the research since 2009. The sheep stem cells have the advantage of being well-tolerated.
Are human trials on the near horizon? The answer is a qualified “yes.”
Human trials might be five years away, Mumaw answers, sooner perhaps in veterinary applications. Beside her, team member Erin Jordan nods agreement. Jordan also attended undergraduate and graduate school at UGA, and presently works at the Regenerative Bioscience Center under Stice. “Stice’s lab is one of the larger on campus,” adds Mumaw. Both Jordan and Mumaw worked in his lab initially.

Erin Tittle Jordan in Dr. Steve Stice’s lab. Also close-up of lab materials. Erin is shown pulling out cells stored in boxes in canes in the liguid nitrogen tank. Colored centrifuge tubes – used to easily visually balance the centrifuge when spinning down samples of cells in media.
Steeped in Science
Despite recent successes, accolades and international headlines the research generated, the two 30-year-old women on the team are nonplussed.
The headlines, they shrug, are only useful if “they show the drive in research and that all of this is to help people; there is nothing more rewarding than helping people and making their worlds better.”
Mumaw, who runs 30-40 miles weekly, lives on a farm in Watkinsville, Ga. While continuing her post-doctoral work, she began veterinary studies this past August. She is training for a half marathon. She tackles running like she tackles a research project: spirited, disciplined and devoted to the work. When she runs, she averages eight miles.
Mumaw’s grandfather was a doctor at Henry Ford Hospital in Michigan and her grandmother a nurse. “My mother taught science. She showed me the effects of acid rain. One of my favorite experiments with her was looking at planarians, the flatworms that are in water. If you cut them in half they regenerate. We added different compounds into their water, to see how it helped their healing.” It was not long before Mumaw realized she was born to be a scientist.
She has two UGA degrees, and is pursuing a third. In the course of the fracture putty experimentations, she discovered she also wants to perform the veterinary surgeries she observed.
Jordan, her colleague and friend, is a research coordinator in Stice’s lab. She has a great deal in common with Mumaw. They are the same age. Both adore animals, and Jordan has adopted five cats from research projects. Both had scientists in the family.
Early on, Jordan too knew she would pursue science and follow in the footsteps of her mother, Sandi Tittle.
Jordan recalls coming to campus with Tittle. “She graduated in the early ‘80s with her BS and then came back later for her Pharm D (doctorate in Pharmacy) and graduated in 2006.” But waiting for her mother to finish her labs didn’t bore her—it fascinated her. Her father became an inspector for the State Department of Natural Resources. With obvious pride, Jordan acknowledges that academic achievement was a family value.
“I had a great interest in science growing up,” she observes.
Today, Jordan has two UGA degrees, a BS in Biology and an MS in Pharmacology.
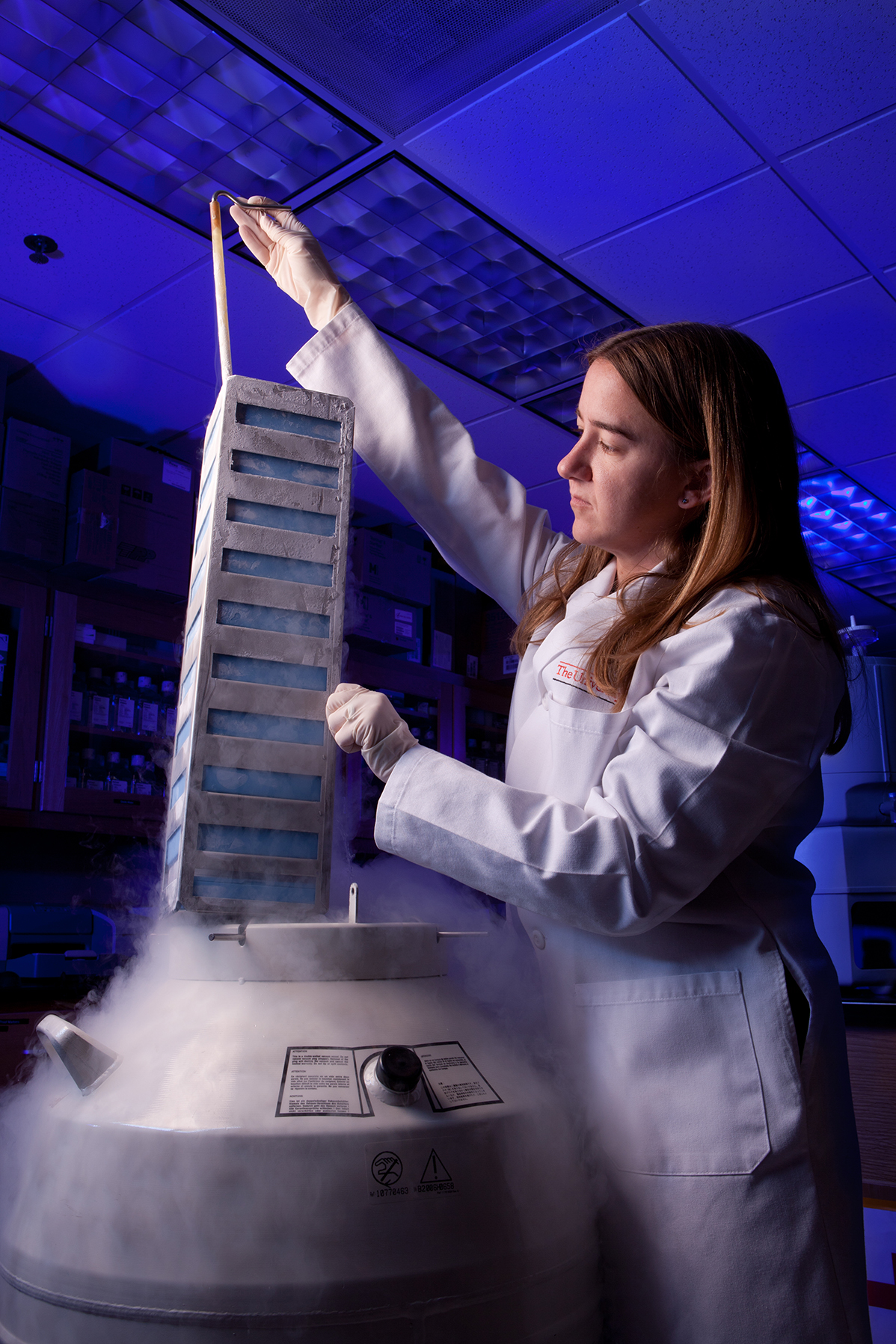
Erin Tittle Jordan in Dr. Steve Stice’s lab. Also close-up of lab materials. Erin is shown pulling out cells stored in boxes in canes in the liguid nitrogen tank. Colored centrifuge tubes – used to easily visually balance the centrifuge when spinning down samples of cells in media.
The Long Road from Research to Clinical Trials
The surgical process of testing the putty was performed twice in 2012. The UGA research team’s “Tried and True Recipe” is one that produces a stable system. This high-tech “recipe” in the developmental stage is expensive, time intensive, and physically exhausting, but it is an exhilarating culmination of the team’s knowledge and abilities. They will refine steps to make the putty economically feasible as they resolve kinks.
Harvesting the sheep cells and preparing the cell culture vital to the experimentations is the recipe the team references. In this case, the two women researchers use some of the nomenclature of a kitchen. In the days leading up to the surgery, they will have performed the work of “plating and transducing” the cells two days prior. “There are probably nine hours of prep work,” Mumaw explains, in creating their recipe.
This kitchen opens exceptionally early. By 4:30 a.m. on the day of the fracture putty experimentations, Mumaw and Jordan are already engrossed in their work inside the Animal Dairy Science building.
Jordan quips that they occasionally get to sleep in until 5:00 a.m. but neither drinks coffee. They both choose caffeine-rich sodas to pry their eyes open, as they will have been in the lab making preparations until late the prior night. Jordan sips a lemon-yellow Diet Mountain Dew and Mumaw drinks Diet Dr. Pepper as they work towards the surgery itself. They describe this laboratory prep time as intense, yet fun.
Although Mumaw and Jordan can prepare the cells earlier, and cryo-preserve them, there still have to be fresh cells on hand the day of surgery. “We will always lose some. When we go to do one experiment for one sheep, we have millions of cells. The cells grow in a monolayer on a plate, so only so many can fit. We balance trying to keep it uncompromised,” Mumaw says.
In the remaining critical hours, they are too busily absorbed for little more than a sip of diet soda. They will grab a “five-or-10 minute break” for yogurt or an apple. Yet they are enthralled by the work.
“We have great fun,” Mumaw smiles as Jordan nods. “We talk; we have to update people.” The research team includes clinical scientists as well as practitioners, all experts in their fields. Getting to spend an entire day together with the research team is exciting, they say, and neither would miss it.
Jordan wouldn’t stay away last summer although she, ironically, had a fracture of her own. “Erin worked on a broken foot!” Mumaw exclaims. “We had a chair to wheel her around in so she could keep working last August.” Among the team members is Dr. Cynthia Trim. In 1987, Trim, a professor emeritus of anesthesiology in the UGA College of Veterinary Medicine, was the first female to become certified in the field of veterinary anesthesiology in the United States.
Trim is a noted expert in both clinical and research anesthesiology. Her job is to be certain the research subject is kept comfortable and calm throughout; she must anesthetize and intubate the subject. “She is an animal advocate,” her team members say. “She puts the animal first.” A technician with a doctorate in marine biology, Merilee Thoresen, assists the team. They refer to Thoresen as “the sheep whisperer.” The concerted effort is to assure the experiment is humanely and immaculately conducted.
Mumaw says the hope is that it will be transferable to other species as well.
“We joke that our liquid nitrogen tanks are like cell petting zoos. We have pigs, sheep, cats, dogs, horses, rats and mice mesenchymal stem cells. We have to work on getting some goats.”

Jennifer Lyn Mumaw with horses
Creating the Recipe: Tried and True
Each fracture putty experiment requires 10 hours of preparatory work by Mumaw and Jordan.
From 10:00 a.m. until 2:00 p.m., the researchers encapsulate cells. Typically, the stem cells are harvested from sheep, though for potential future applications cells have also been harvested from horses.
Next, from 2-3:00 p.m., the researchers centrifugally wash the cells to eliminate the growth media. This usually produces three milliliters with 1.5 trillion cells, the amount necessary to perform six fracture putty injections.
Does “the recipe” ever go tragically wrong? They laugh hard. Mumaw, the senior team member, says, “Luckily we were able to recover because we had a spare set. We had harvested the cells for hours; counted them, encapsulated them, but it had gone wrong. But, we had cells cryopreserved and used them.”
At 3:00 pm, the following hour, Dr. Peroni performs the first of three sheep surgeries. He will typically perform two to three surgeries each day in a given week.
Both Mumaw and Jordan assist with post-surgical care of the sheep. By 7:00 or 8:00 p.m., the women go home, only to return before 5:00 a.m. on the transduction day to prepare for the next surgery. Two weeks later, the team can evaluate the outcomes aided by radiographs of the injected defect. For Jordan, “that is the best part.”
Often the sheep used are from a UGA-run farm. Both women love the sheep, and report their subjects recover comfortably in their stalls, fully attended. The sheep are able to put full weight upon the fractured limb immediately. For the integrity of the experiment, it is critical the sheep are closely monitored, protected from injury or disease. Dr. Trim is key to oversight of the subject’s comfort and well-being throughout surgery and after. The team evaluates the subject at the systemic level, to analyze if the recipient of the fracture putty has accepted the therapy.
The Rocky Road to Research Gold
“We’ve had a lot of success and know we have pitfalls to work out,” says Mumaw one morning as she describes the issues of funding and other hindrances. The matter of human clinical trials, eagerly anticipated by anyone who has heard of the fracture gel, is excruciatingly slow of necessity. Mumaw, who has a fresh, unworried face, says airily that she has been doing cell culture for 12 years. “We have to prove a lot of safety and efficacy beforehand,” she stresses.
There are the not-so-pleasant aspects of long research: problems of inconsistency. Grinding tedium and long hours are normal. But the two young researchers seem completely undeterred.
Cryogenic preservation of prepared cells will make the putty financially feasible. “We will make it, have it ready to go, and then put it into a freezing process. It can then be transferred around the world on dry ice for surgeries, shipped straight to (medical facilities) in stock containers.”
The dream outcome, the two women agree, is “To help people. To transform medicine.” They dream of helping people heal better and faster, especially those for whom there is often no option but amputation. Both Mumaw and Jordan especially think of injured soldiers returning from combat. “It could help anyone,” Jordan muses. In November of 2012, they presented in Savannah with principal investigators Stice and Peroni at the Society of Regenerative Medicine.
“Sometimes the research doesn’t translate well to humans or large animals,” says Mumaw. “We didn’t have the same translation of the results when we went from rodents to large animals. You have complicating interactions with all the systems in the body. Is it a problem with the polymer, the gene, or an immune response? Knowing which direction to go is a little astounding; you can’t test all of them at once.”
Confounding frustration is a scientist’s norm. But Jordan explains these are the times when the great triumphs, eureka moments, arise. And the joy of discovery is shared by the entire research team.
Mumaw adds succinctly, as Jordan nods, “The last experiment showed the problems were what we thought they were. Now we know where those problems are. We will address that through some new routes.”
And, by George, they may only be one Diet Mountain Dew, one Diet Dr. Pepper away from triumph!